فهرست مطالب
The Journal of Tehran University Heart Center
Volume:14 Issue: 2, Apr 2019
- تاریخ انتشار: 1397/12/23
- تعداد عناوین: 9
-
-
Pages 47-52BackgroundPercutaneous coronary intervention (PCI) of total chronic coronary occlusions (CTOs) still remains a major challenge in interventional cardiology. There is little knowledge in the literature about differences in CTO-PCI between diabetic and nondiabetic patients in the era of third-generation drug-eluting stents (DESs). In this study, we analyzed the impact of diabetes mellitus (DM) on procedural characteristics, complications, and acute outcomes in a cohort of 440 patients.MethodsBetween 2012 and 2016, we recruited 440 consecutive patients, 116 of them with DM. All the patients underwent PCI for at least 1 CTO. Antegrade and retrograde CTO recanalization techniques were applied. Only third-generation DESs were used. We used t-tests and the Pearson chi-quadrat test to test the significant differences in the variables between the 2 groups.ResultsThe patients with DM were older than the nondiabetics (64.5 y vs. 61.1 y; P=0.003), and they suffered more frequently from a chronic kidney disease (7.1% vs. 2.4%; P=0.001). The nondiabetics less frequently had arterial hypertension (75.3% vs. 89.7%; P=0.001); however, they more often had a family liability for CAD (32.1% vs. 22.4%; P=0.050) and had a higher left ventricular ejection fraction (59.2% vs. 56.7%; P=0.011). The success rate was 85.2% in the patients without DM and 81.2% in the patients with DM (P=0.403). The existence of DM had no impact on the procedural success and complication rates.ConclusionOur study on 440 patients shows that diabetics and nondiabetics have similar success and complication rates after the recanalization of CTOs using third-generation DESs. It is a feasible and safe procedure and can be recommended as an alternative treatment.Keywords: Coronary artery disease, Coronary occlusion, Diabetes mellitus, Treatment outcome
-
Pages 53-57BackgroundPercutaneous coronary intervention (PCI) has become the first-choice treatment strategy the world over for patients with chronic coronary artery disorders. This study compared the effects of previous PCI procedures on the short-term postoperative results of coronary artery bypass graft surgery (CABG).MethodsThis cross-sectional analytical study recruited 220 patients who underwent CABG in Afshar Hospital in the Iranian city of Yazd between March 2009 and February 2013. The mean postoperative morbidity and mortality rates, the mean postoperative left ventricular ejection fraction (LVEF), the mean hemorrhage volume, the mean serum urea level, and the mean length of stay in the intensive care unit (ICU) were compared between the PCI and non-PCI groups.ResultsAmong the 220 participants, 147(66.8%) were male and 73(33.2%) were female. The mean age of the study population was 59.41±10.52 years. There was no significant difference in the risk of mortality between the 2 groups (P=0.369). The mean serum urea level was 21.14±6.52 mg/dL in the PCI group and 14.45±1.08 mg/dL in the non-PCI group (P=0.016). The mean postoperative LVEF was 43.19±8.81% in the PCI group and 45.51±8.15% in the non-PCI group (P=0.044). The mean length of stay in the ICU was 3.34±1.23 days in the PCI group and 2.22±0.56 days in the non-PCI group (P<0.001). The mean hemorrhage volume was 1113.01±428.13 mL in the PCI group and 961.42±228.31 mL in the non-PCI group (P=0.027).ConclusionPrevious PCI procedures did not affect the post-CABG mortality rate; however, some postoperative results were worse in the PCI group than in the non-PCI group, which should be considered before the selection of the revascularization method.Keywords: Coronary artery disease, Angioplasty, balloon, coronary, Percutaneous coronary intervention, Coronary artery bypass
-
Pages 59-66BackgroundDevelopment of contrast-induced acute kidney injury (CI-AKI) in patients with ST-elevation myocardial infarction (STEMI) treated via primary percutaneous coronary intervention (PCI) is a major cause of morbidity and mortality worldwide. The neutrophil-to-lymphocyte ratio (NLR), which is a marker of inflammation, has been demonstrated to be associated with the development of major adverse cardiovascular outcomes in many studies. From this point of view, in this study, we aimed to evaluate the predictive value of the NLR as regards the occurrence of CI-AKI in patients with STEMI undergoing primary PCI.MethodsThis study was conducted at Dr. Siyami Ersek Training and Research Hospital from May 2008 to June 2016. A total of 2000 patients with STEMI treated via primary PCI were enrolled in the study. The NLR was calculated as the ratio of the number of neutrophils to the number of lymphocytes. All venous blood samples were obtained within 8 hours after admission. CI-AKI was the primary end point of the study. Then, the relationship between CI-AKI and the NLR was assessed.ResultsCI-AKI was detected in 148 (7.4%) patients. The patients who developed CI-AKI had a significantly higher NLR than those who did not (7.08±4.43 vs. 6.18±3.98; P=0.011). In the multivariate logistic regression analyses, the NLR remained a significant independent predictor of CI-AKI (OR: 1.78, 95% CI: 1.21–2.61, and P=0.003).ConclusionThe NLR may be a significant independent predictor of CI-AKI in patients with STEMI treated via primary PCI and higher NLR values could be independently associated with a greater risk for CI-AKI.Keywords: Acute kidney injury, Myocardial infarction, Percutaneous coronary intervention, Neutrophils, Lymphocyte count
-
Pages 67-73BackgroundPostoperative cognitive decline is a common complication observed frequently after general anesthesia in the immediate postoperative phase. We studied the effects of dexmedetomidine versus midazolam during coronary artery bypass graft (CABG) surgery on cognitive and memory function.MethodsIn this clinical trial, 42 elective on-pump CABG candidates under general anesthesia, aged between 40 and 65 years, were enrolled randomly in 2 groups. Group A received 0.05–0.1 mg/kg of midazolam and Group B received 1 µg/kg of dexmedetomidine. One day before surgery, all the participants underwent the Persian version of the Mini-Mental State Examination (MMSE) and the Persian version of the Wechsler Memory Scale (WMS) test for a comparison of cognitive impairment and memory functions. Both groups were given fentanyl and propofol for the induction of anesthesia and muscle relaxants. The MMSE and WMS tests were repeated 5 and 30 days after surgery.ResultsThe mean±SD of age was 55.47±7.18 y in Group A and 55.39±6.08 y in Group B. Eighty percent of the participants were men in both groups. There were no significant differences between Group A and Group B in the MMSE and WMS before surgery (89.04±14.30 vs. 97.10±18.10, respectively; P=0.059), but the WMS was significantly different 30 days after surgery (87.60±14.30 vs. 103.53±19.93, respectively; P=0.005). Group A showed high cognitive impairment and low WMS scores compared with Group B (P=0.005). Additionally, the MMSE results were not statistically different between the 2 groups postoperatively (24.80±3.18 vs. 23.55±4.18, respectively; P=0.394).ConclusionOur results showed that dexmedetomidine might have a lower impact on cognitive function than might midazolam among patients undergoing CABG.Keywords: Cognitive dysfunction, Coronary artery bypass, Dexmedetomidine, Midazolam
-
Pages 74-80BackgroundAcute hypoxemia is the main characteristic of acute respiratory distress syndrome (ARDS), which is one of the most critical complications of coronary artery bypass grafting (CABG). Given the dearth of data on acute hypoxemia, we sought to determine its prevalence and risk factors among post-CABG patients.MethodsThis cross-sectional study was conducted on on-pump CABG patients in Tehran Heart Center in 2 consecutive months in 2012. The effects of arterial blood gas variables, age, gender, the duration of the pump and cross-clamping, the ejection fraction, the creatinine level, and the body mass index on the prevalence of hypoxemia at the cutoff points of ARDS and acute lung injury were assessed.ResultsOut of a total of 232 patients who remained in the study, 174 (75.0%) cases were male. The mean age was 60.60±9.42 years, and the mean body mass index was 27.15±3.93 kg/m2. None of the patients expired during the current admission. The ratio of partial pressure arterial oxygen to the fraction of inspired oxygen (PaO2/FiO2) 1 hour after admission to the intensive care unit (ICU), before extubation, and at 4 hours after extubation was less than 300 mmHg in 66.6%, 72.2%, and 86.6% of the patients and less than 200 mmHg in 20.8% 17.7%, and 30.2% of the patients, respectively. Among the different variables, only a heavier weight was associated with a PaO2/FiO2 ratio of less than 300 mmHg at 1 hour after ICU admission and at 4 hours after extubation (P=0.001). A rise in the cross-clamp time showed a significant association with the risk of a PaO2/FiO2 ratio of less than 200 mmHg at 4 hours after extubation (P=0.014).ConclusionThis study shows that hypoxemia following CABG is very common in the first 48 postoperative hours, although it is a benign and transient event. The high prevalence may affect the accuracy of the ARDS criteria and their positive or negative predictive value.Keywords: Risk factors, Hypoxia, Coronary artery bypass, Respiratory distress syndrome, adult
-
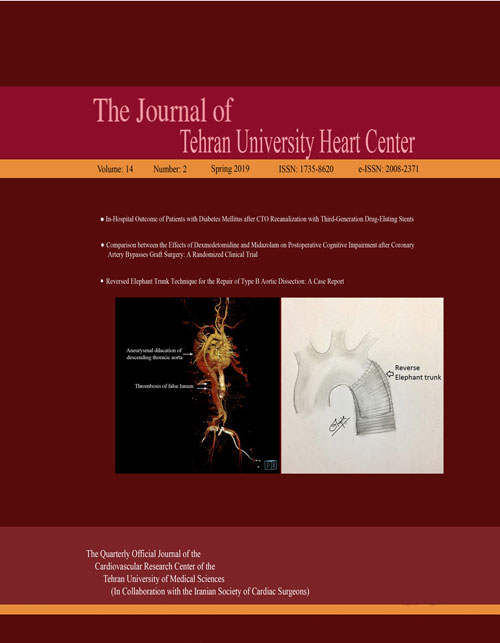
Pages 81-84We report a case of a type B aortic dissection with an aneurysm treated by the replacement of the proximal descending thoracic aorta via the reversed elephant trunk technique. A 48-year-old asymptomatic man was diagnosed with a type B aortic dissection, moderate aortic regurgitation, and a good biventricular function in March 2012. Four years later (April 2016), a contrast-enhanced computed tomography examination revealed an aneurysmal dilatation in the patient’s descending thoracic aorta with a thrombosis in the proximal part of the false lumen, which warranted surgical repair. He underwent type B aortic dissection repair through the left posterolateral thoracotomy. Three months after the surgery, the patient developed a type A aortic dissection with severe aortic regurgitation, which was successfully managed via a Bentall procedure with arch replacement facilitated by the reversed elephant trunk technique performed during the initial surgery through thoracotomy. At 2 years follow-up, the patient was doing well with a normal left ventricular function.Keywords: Dissection, Aortic aneurysm, thoracic, Thrombosis
-
Pages 85-89Transcatheter aortic valve implantation (TAVI) has shown favorable outcomes in patients with severe symptomatic aortic valve stenosis who are at high surgical risk or who are unsuitable candidates for open-heart surgery. However, concerns exist over treating patients who have undergone previous mitral valve surgery due to the potential interference between the mitral prosthetic valve or ring and the TAVI device. In this case report, we present a case in which a patient with symptomatic severe aortic stenosis and previous mechanical mitral valve replacement was successfully treated with TAVI using a Portico valve, which is under-researched.Keywords: Aortic valve stenosis, Transcatheter aortic valve replacement, Mitral valve
-
Pages 90-91An 82-year-old female patient presented with complaints of dyspnea and increasing palpitations caused by food reflux. There was no risk factor except hypertension. On physical examination, the heart rate was 120 beats/min and arrhythmic and blood pressure was 130/80 mmHg. Electrocardiography showed high-rate atrial fibrillation. Laboratory parameters were unremarkable. Echocardiography illustrated a hyperechogenic and well-circumscribed mass, 40×55 mm size, in the posterior left atrium (Figure 1, Video 1). The mass size increased with breathing and the Valsalva maneuver. There was no pathology on chest radiography. The atrial fibrillation returned to sinus rhythm spontaneously, but paroxysmal atrial fibrillation attacks were observed, which were related to food reflux at follow-up. Subsequently, cardiac computed tomography, performed to determine the etiology, failed to demonstrate any pathological findings involving the left atrium. However, there was a sliding hernia in the paraesophageal region compressing the left atrium from the inferior-posterior region (Figure 2). Hiatal hernia surgery was recommended on account of the intermittently repeating symptoms. The patient refused the operation, and she is under follow-up with medical treatment. Hiatal hernias are described as abnormal protrusions of the stomach through the diaphragmatic esophageal hiatus. They are usually latent, with symptoms often related to gastroesophageal reflux signs. Huge hernias can rarely be misdiagnosed as intracardiac masses during echocardiography. Additionally, they can cause paroxysmal atrial fibrillation attacks due to symptomatic left atrial compression and the irritation of the vagus nerve. Huge hiatal hernias may mimic cardiac masses and rarely may cause paroxysmal atrial fibrillation attacks, as was the case in our patient. They should, be carefully differentiated from other cardiac pathologies.Keywords: Hernia, hiatal, Heart atria, Atrial fibrillation
-
Pages 92-93A 54-year-old woman was admitted to our hospital with a fever of 1 week’s duration and a distal embolic event 4 days previously in the second and third digits of her right hand. She had a history of aortic valve replacement (STj#19) 2 months earlier as well as mitral valve replacement (STj#26) and tricuspid valve repair 10 years before. Lab data showed an increased white blood cell count and an elevated erythrocyte sedimentation rate. Blood culture was positive only in 1 round with Pseudomonas aeruginosa growth, which was not compatible with the patient’s good general condition. Transthoracic and transesophageal echocardiography, abdominal sonography, and computed tomography (CT) scan of the right hand were unremarkable. The patient was treated for infectious endocarditis with antibiotics for 6 weeks and then discharged. On follow-up transthoracic echocardiography, 1 month after discharge, an echo-free space in the posterolateral wall of the ascending aorta was detected. The second transesophageal echocardiography was highly suggestive of a pseudoaneurysm in the ascending aorta (Figure 1A & Video 1), which was subsequently confirmed by a CT angiography of the ascending aorta (Figure 2). For a better evaluation, aortography was done and it revealed a pseudoaneurysm in the posterolateral wall of the ascending aorta (Figure 3 & Video 2). A review of the previous transthoracic and transesophageal echocardiography images demonstrated that this pseudoaneurysm had been missed because it was filled with a thrombosis (Figure 1B & Video 3). The ascending aorta was normal in aortography before the second surgical operation. It appears that the most probable scenario was thrombosis formation in an iatrogenic aortic pseudoaneurysm at an unusual site, causing such presentations. The thrombosis was resolved with meticulous anticoagulation, leading to the clarification of the pseudoaneurysm. The administration of an anticoagulant was obligatory in this patient because of the presence of 2 mechanical valves. Nevertheless, this administration could lead to catastrophic events such as a ruptured ascending aorta, so the early detection of this complication may reduce the risk to the patient and confer an appropriate treatment. We repaired our patient’s pseudoaneurysm via surgery, and she was discharged in good physical condition. The development of an aortic pseudoaneurysm is an uncommon complication of open-heart surgery, and it usually forms in the anterior wall; nonetheless, its formation in the posterior wall is rare and can be due to the deep cannulation of the ascending aorta during surgery. The presence of this complication should, therefore, be kept in mind by any cardiologist who encounters a patient with an embolic event and previous cardiac surgery.Keywords: Aorta, Aneurysm, false, Echocardiography, Diagnosis